
Obstructive sleep apnea hypopnea syndrome (OSAHS) is a comprehensive name to identify sleep disordered breathing. Sleep apnea occurs when an individual ceases to breathe periodically throughout the night. Hypopnea involves slow and shallow breathing, causing airway pressure to decrease by half, which leads to low oxygen levels in the blood (desaturation). When you have a decrease in air intake and not a cessation of breathing, you have hypopnea, not sleep apnea.
The Relationship Between Sleep Apnea and Sleep Hypopnea
Understanding the relationship between sleep apnea and hypopnea can be complex. They are often mentioned together as if they are the same disorder. Also, the new term for the disorder, OSAHS, includes both types of disordered breathing, even when one can occur without the other.
A couple of decades ago, not much was understood about the relationship between sleep apnea and hypopnea, and hypopnea was not fully defined. Thanks to research, it is now understood that sleep apnea and hypopnea are two types of disordered breathing in which both result in a decrease in oxygen flow to the lungs.
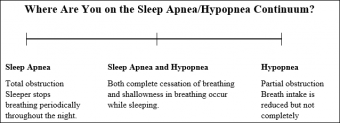
It is possible to have both sleep apnea and hypopnea breathing together, or to have just sleep apnea or sleep hypopnea separately. The easiest way to understand the disorder is to view it as a continuum. Some people have just hypopnea (shallow breathing), and some sleep apnea (interruption/cessation in breathing), and some have both types of disordered breathing.
Effects and Symptoms
Hypopnea is associated with a decrease in the oxygen saturation of the blood up to 4 percent during sleep due to a decrease in the amount of air breathed. This is usually caused by a partial block in the airway. Without the proper amount of oxygen in the blood, the body's organs do not get enough oxygen to function properly.
The effects of decreased oxygen could lead to:
- Disruptive sleep patterns
- Inability to concentrate/poor memory
- Fatigue/lethargy
- Irritability
- Headaches
If hypopnea is allowed to continue long-term, it could contribute to more severe health consequences, such as:
- Heart disease
- Heart attack
- Stroke
Why You Are Tired
When you suffer from this sleep disorder, your body does not get enough oxygen while sleeping. The brain recognizes this and in an effort to improve the situation, the brain jolts the body awake just slightly. It is just enough movement to get the airway back open so you are getting a better flow of oxygen.
The problem here is that this happens several times per night. The brain never goes through the sleep cycles it needs and you remain constantly tired.
Causes
According to the New York Times in-depth report on obstructive sleep apnea/hypopnea, there are factors that could contribute to the development of disordered breathing while sleeping.
- Soft tissues in the mouth and throat might not fully collapse, causing a partial block that will partially restrict breathing
- Wider neck circumference
- Overweight
- Structural abnormalities in the chin, skull, tongue, or jaws
- Smoking cigarettes or drinking alcohol
- Medical conditions such as diabetes, gastroesophageal reflux disease (GERD), and Polycystic Ovary Syndrome (PCOS)
Diagnosis
Recognizing sleep apnea and hypopnea can be difficult because the person may be aware of no other symptoms besides excessive daytime sleepiness. A sleep study can detect the nighttime breathing disorders, and an apnea hypopnea index can measure the severity of the condition.
Full Sleep Study
During the sleep study, a number of tests will be performed to detect whether or not you have a breathing problem during the night and why it is occurring.
A full sleep study uses devices, such as electroencephalogram (EEG), to measure:
- The amount of pressure your breath intake produces
- The temperature and pressure in your sinuses
- The amount of carbon dioxide you are breathing out
- Your oxygen levels (oxygen saturation test)
Your sleeping posture, heart rate, and the pH balance in your esophagus might be assessed. The physicians might also want to record you while you are sleeping.
The Apnea Hypopnea Index and the Respiratory Disturbance Index
During your full sleep study, your physician will use instruments of measure, such as the Apnea Hypopnea Index and the Respiratory Disturbance Index, to understand the type and frequency of your disordered nighttime breathing.
The Apnea Hypopnea Index
- The Apnea Hypopnea Index divides the number of hypopneas and apneas into the number of hours the patient sleeps. For example, if a person sleeps eight hours and experiences 40 apneas and 60 hypopneas, the AHI value is 12.5, which would be a mild case.
- AHI values measure the severity of the sleep problem:
- Five to 15 are mild
- 15 to 30 are moderate
- Higher than 30 is severe
The basic calculation aside, differences in measuring hypopnea and apnea can alter the results. To approach this problem, in September, 2013, the AASM defined standardized criteria for the measurement of hypopnea. The preferred method is to include whether or not the patient is partially aroused from sleep.
Respiratory Disturbance Index
The Respiratory Disturbance Index (RDI) is a measurement that includes hypopneas and apneas in its calculations. In addition, RDI also include other sleep disturbances the sleeper may experience throughout the night, including:
- Hypoventilation
- Desaturation
- Snoring arousal
Since this measurement includes arousals that are not necessarily hypopneas or apneas, the RDI measurement may be higher than the AHI, according to CPAP Talk.
Treatment
Most commonly, reducing weight can help to improve sleep apnea symptoms, especially in individuals who have a large amount of tissue around the neck region. Some surgeries are available to remove excess tissue at the back of the throat triggering the episodes. However, surgery is often used as a last resort and only if a physical aspect can be altered to improve the outcome of the hypopnea or apnea.
Treatment may also include the use of a Continuous Positive Airway Pressure (CPAP) device. This device will keep a continuous flow of air coming into the air passageway to keep it open. It fits snuggly over the nose and/or mouth. The pressure in these devices is adjusted so that the tissues surrounding the air passageway is kept pushed open, but not so much that it keeps you from breathing regularly. For many patients, although the first use of a CPAP mask or device can be uncomfortable; the quality of sleep obtained is excellent.
Difficulties Breathing During the Day
According to MedlinePlus, breathing irregularities are not usually cause for concern. However, some conditions might cause breathing difficulties during the day and night, such as asthma, pneumonia, neuromuscular conditions, and lung disease.
If you have one of these conditions and you are having trouble breathing during the daytime, or if you have sudden difficulty breathing and it does not go away, immediate medical attention is necessary.
When to Get Help
Even though people often have the disorder for years before they obtain help, it is important to seek help for hypopnea. Like sleep apnea, hypopnea has serious short-term and long-term consequences if left untreated.
Loud snoring, daytime sleepiness and tiredness might be your only signs of sleep disordered breathing. If you find you cannot get a good night's sleep, seeking help from your physician and obtaining a referral to a sleep clinic will be worth it. If anything, they could help you with your sleeping arrangement to get a better night's sleep, even if you do not have hypopnea.







